Osteochondrosis is a chronic recurrent disease that occurs in the context of continuous destruction of vertebrae and intervertebral discs.They distinguish between breasts, lumbar pathology, and neck according to the location of vertebrates undergoing degenerative changes.The main symptom of osteocartilage degeneration is pain, and its severity increases during physical fatigue and stiffness in exercise.In clinical cases, there are usually signs of vertebrae: headache, blood pressure jumps, reduced vision and hearing.
Diagnosis is based on the results of instrumental studies - X-ray, MRI, CT.In the treatment of osteochondrosis, various clinical and pharmacological groups are used.To improve its clinical efficiency, physical therapy and massage procedures were performed.One of the main methods of treatment and prevention is physical therapy exercises.
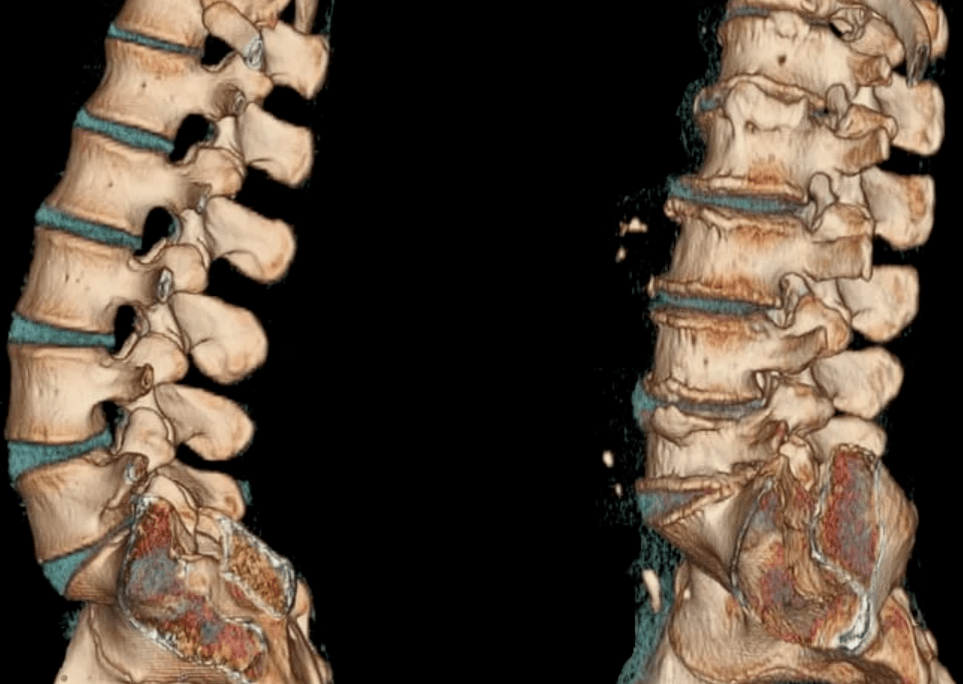
Disease development mechanism
The pathogenesis of osteochondrosis is based on the core loss of its hydrophilic properties.The semi-fluid structure consists of connective tissue fibers and a jacket.As people grow, the blood vessel passages of each intervertebral disc between the vertebrae drop.The nutrient intake is scattered, that is, according to the principle of spontaneous concentration.This explains the possibility of not being able to fully recover cartilage tissue after an injury or overworking on the spine.
The process of osteochondrosis exacerbates changes in hormonal background and imbalanced diets.Nutritional amounts that are sufficient to make their full function do not enter the cartilage tissue, which can cause the following diseases of its structure and properties:
- Strength and elasticity disappear;
- Form, consistency, and configuration changes.
The intervertebral disc is flat and radial cracks form in the annulus of fibrous fibres.This results in a decrease in distance between adjacent vertebrae.The connective tissue of the annulus and ligaments gradually participates in the pathological process.In response to tissue decay, the immune system begins to produce immunoglobulins, resulting in sterile inflammation and edema formation in the joints of nearby joints and soft tissues.The capsules of the joint are stretched, so the disc stops reliably fixing the vertebrae.With instability of the intervertebral segment, the likelihood of nerve roots or vascular compression increases.This usually occurs in the cervical osteocartilage and causes its obvious symptoms.
Causes and provocative factors
In the state of the intervertebral disc, the reduction in tone of the spinal skeletal muscles can adversely affect.The irrational, asymmetrical function of the muscles is in non-physiological positions for a long time, for example, when working on a computer, the head lowers the head.Constantly wearing a heavy bag on your shoulder, a dream on your soft mattress and a high pillow can cause damage to the cartilage fabric.
The following external and internal negative factors also accelerate the destruction of the intervertebral disc:
- endocrine and metabolic disorders;
- infectious pathology, especially chronic diseases;
- anterior spinal injury (compression fracture, bruising);
- Often hypothermia;
- Systemic or degenerative nutritional diseases, psoriasis, rheumatoid arthritis, osteoarthritis, osteoporosis.
If a person has bad habits, he is in danger.Smoking and alcohol abuse can worsen the vascular state, leading to insufficient blood circulation and a lack of nutrients in the cartilage tissue of the intervertebral disc.
In the presence of flat feet or clubs, the risk of osteochondrosis of any positioning is greatly increased.This congenital or inherited defect becomes the cause of increased spinal load because it is impossible to ensure proper depreciation of support.Obesity is the factor that occurs in pathology.
As fat tissue is deposited in various parts of the human body, the support for balance is complex, which can lead to the effect of excessive load on intervertebral joints.
Clinical pictures
The first clinical manifestation of cervical, chest or lumbar osteochondral disease is back pain.During the recurrence, it penetrates into nearby parts of the body.Minimal exercise leads to an increased severity of pain syndrome.A person's reaction is to adopt a compulsory position where the intensity of uncomfortable feeling is very little:
- People with cervical osteochondrosis would rather not turn their heads but their entire body.
- With breast pathology, a person is even afraid to hold his breath completely because this becomes the cause of acute pain in the chest area.
- Due to the erosion of the spinal nerves, it is difficult to sit down, get up and walk away.
Most patients complain to their doctor about the stupid constant pain and the restricted sense of movement in the morning.This requires other differential diagnoses to rule out myositis (an inflammatory process of back skeletal muscle) and osteoarthritis.The reason for pain is that stress pain is the affected vertebrae movement segment of the muscle tissue compensating stress stability.Constant pain syndromes of weak or moderate severity also occur due to the significant range of the disc and the development of sterile inflammation.
For specific localized osteocartilage, specific symptoms are characteristic.For example, with lumbar pathology, lumbar behavior often occurs – pain attacks on the lower back and back of the thigh.Visceral pain in the heart area, right lower cartilage, stomach, numbness, increased skin sensitivity, tightening in the vertebrae, clinically manifested sternum osteochondral disease.However, the most obvious and diverse symptoms are distinguished by the pathology that affects the cervical disc.
Due to the displacement of the vertebrae, bone plants form, the vertebral arteries are compressed to supply brain cells, thus providing them with oxygen.A person violates coordination of exercise, noise in the ears, headaches, arterial hypertension.
What will happen without treatment
Most complications of osteochondrosis occur due to the formation of hernia in the intervertebral disc.When this vertebral structure is displaced, it forms, resulting in a rupture of the posterior longitudinal ligament.The disc becomes more unstable, with part of it protruding to the cerebrospinal tract.If during the formation process, its purpose core penetrates into the passage, it is considered that the hernia is considered to be an explosion.
This pathological state of vertebrates is prone to compress the development of spinal cord and discoid myelopathy.Clinically, it shows its own manifestations, weaknesses in the muscle groups of certain legs or arms, paralysis, muscle atrophy, and changes in tendon reflexes.Diseases that empty the bladder and/or intestinal tract can also be observed.Due to the formation of a vertebral hernia, the arteries feeding the spinal cord are squeezed.The ischemic region forms where all nerve cells are killed.The appearance of SO is known as a neurological defect - a movement violation, a reduced sensitivity, and Trothy is frustrated.

Treatment strategies
Osteochondrosis does not completely cure itself because no drugs have been synthesized so far, and its intake will help restore damaged discs and vertebrae.But treatment options must include cartilage protectors - slow-acting symptom drugs.Priority is given to drugs containing active chondroitin components of sulfate and/or glucose sulfate (hydrochloride).
The clinical effectiveness of these drugs has been confirmed by years of research results.With the prolonged period of admission (from 3 months to 2 years), partial regeneration of cartilage tissue, as well as other connective tissue structures - ligaments, tendons, Burns.When they accumulate in the intervertebral discs of glucose and chondroitin, they begin to exert obvious analgesic, inflatable, anti-inflammatory effects.This allows you to reduce the dose of NSAID, glucocorticoids, muscle relaxants, thereby reducing the pharmacological load in the body.
When significant damage to cartilage tissue is observed, irregular use of articulatory drugs or drugs used to treat osteocartilage are ineffective.
To eliminate symptoms that usually occur in cervical or breast oschondrosis, medications are used to improve blood circulation, nootropics, a drug that improves microcirculation in the maze of vestibular instrument pathology.
If necessary, antidepressants, anticonvulsants are included in the treatment regimen.
In the treatment of osteochondrosis, physical therapy methods are used: UHF therapy, magnetic therapy, and laser therapy.Use reflexology, massage, exercise therapy, rest therapy, swimming, yoga.Due to the ineffectiveness of conservative treatment, the patient underwent surgical intervention.Disks, which are laser reconstructions or implant replacements to practice.
































